Blog Post by Coach JulieNCI Certified Nutrition Coach L1 & Certified Mindset Coach  Do you suffer with Rheumatoid Arthritis? Rheumatoid arthritis (RA) is an autoimmune and inflammatory disease. Symptoms of this disease are tender, warm or swollen joints, joint stiffness, fatigue, fever and loss of appetite. Early symptoms tend to appear in the smaller joints first, usually hands and feet. RA symptoms can wax and wane in severity including periods of remission and alternatively periods of increased intensity, called flared. Long term effects of this disease can cause your joints to deform and shift out of place. Western medicine admittedly states they are not sure what causes RA. They state they believe there is a genetic component, but that genes don’t actually cause the issue. This is something that I have been trying to teach my clients and audience, genes don’t cause or create a diseased state in your body. Just because your parents have diabetes does not mean that you’re doomed to have diabetes. If that’s how disease worked, you would have diabetes when you were 7. It wouldn’t wait until you were 37. Genetics may make you more predisposed to a certain disease or condition, but environmental factors have to be present to trigger and activate that disease. Your genetics load the gun, but your lifestyle and environment pull the trigger. This is why it is important to manage your health and wellness throughout your life and prior to symptoms appearing. Usually if you wait for symptoms to appear, the disease is already present. Studies are suggesting that there may be a link between Rheumatoid Arthritis (RA) and gut health. I can’t say that I’m surprised by this. RA is an autoimmune disease and an inflammatory disease. The root cause of many autoimmune diseases is inflammation and inflammation usually comes from the gut. This is where the environmental factors we spoke about above come into play. These studies are specifically referring to low stomach acid causing flares of RA. When stomach acid is low, usually people will experience food-allergy symptoms which can show up as RA pain. Stomach acid helps break down proteins in your stomach so that the intestines can absorb it. Without adequate stomach acid, your intestines absorb partially broken down protein which causes allergies. Signs of low stomach acid are: abdominal pain, bloating, gas, diarrhea, constipation, undigested food in stool, reflux and heartburn. Yes, you read that right, reflux and heartburn are signs of low stomach acid, not too much acid. If you struggle with RA, you may see some relief by looking at your gut health and working to optimize gut health. Avoid proton pump inhibitors (PPIs) like Prilosec or Nexium as they will lower your stomach acid. Some RA sufferers have stated that there are RA drugs that have caused acid reflux issues and therefore they have been prescribed a PPI to help them manage. It is very important to talk to your doctor about other options. Perhaps a change in your RA medication would be an option. If not, I would suggest doing some stomach acid tests to see if the issue you are experiencing is actually high stomach acid. If it isn’t, you have other options. If you are experiencing low stomach acid, you could find relief from your stomach acid issues but supplementing with Betaine HCL and adding stomach acid to your gut to help you break down food. This would not only eliminate the PPI and the symptom, but it would help you break down food and could potentially lessen the frequency and intensity of RA flares.
0 Comments
What is PCOS - Polycystic Ovary Syndrome is a hormonal disorder that affects millions of women.2/4/2023 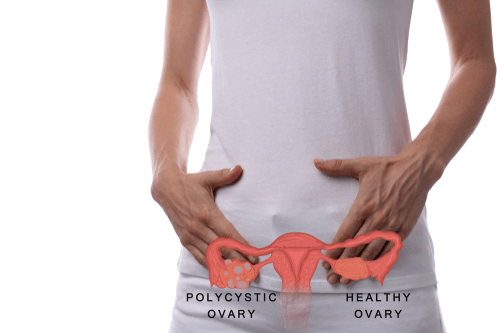 Polycystic ovary syndrome (PCOS) is a condition affecting between 1 in 10 and 1 in 20 women of childbearing age. This condition causes the body’s hormones to become unbalanced, leading to issues like ovarian cysts, increased hair growth on the face and body (hirsutism), acne, weight gain or obesity, thinning hair, irregular menstrual periods, and even infertility. It’s very likely you or someone you are close to suffers from PCOS. You must have two of the three following criteria to be diagnosed with PCOS : Irregular Periods Hyperandrogenism (Higher Testosterone) Polycystic Ovaries About 50% of people who have PCOS also suffer from obesity. Being diagnosed with PCOS is not a “death” sentence when it comes to being able to lose weight. Thankfully, more and more doctors are beginning to recognize the importance diet plays in preventing and controlling PCOS. Insulin is thought to play a major role in PCOS. This powerful hormone, released by the pancreas, exists to transport sugar out of the blood and into the cells. However, many women with PCOS are insulin resistant, meaning this process doesn’t work correctly within their bodies. As a result, high levels of insulin contribute to many of the symptoms of PCOS, such as weight gain, high cholesterol, diabetes, and ovarian cysts. Ladies, you’ll be glad to hear that controlling your diet can play a huge part in helping reverse insulin resistance. Firstly, stick to a balanced diet consisting of whole grains, fruit and vegetables, healthy fats, and protein. Losing just 5% to 10% of body weight can improve symptoms of PCOS and reduce insulin resistance. Physical activity has been shown to play an important, if not essential, role in the treatment and prevention of insulin insensitivity, meaning it’s central to the management of PCOS. At least 30 minutes of aerobic activity is recommended a week. Aim for strength training twice a week, as in order to improve insulin levels and aid weight loss, lifting weights is thought to be an important aspect of exercise for those with PCOS. Let’s have a look at the best dietary choices to decrease insulin resistance and therefore manage PCOS symptoms. While standard guidelines recommend that we get 45% to 65% of our daily calories from carbohydrates, women with PCOS should strive for the lower end of this range. If you’re already insulin resistant, a lower carb diet is typically a better option. I promise you won’t have to starve yourself to get the benefits of a lower carbohydrate intake. Even switching to a diet consisting of 43% carbohydrates has been shown to reduce fasting insulin levels, and therefore improve insulin sensitivity, in women with PCOS. Choose high fiber, whole grain carbohydrates like brown rice, oatmeal, whole rye, and whole wheat pasta in small amounts. Not only do whole grains have a lower GI rating, which improves insulin sensitivity, but they also help improve cholesterol levels – another PCOS-related complication. And don’t forget the vegetables. These are always your best source of carbohydrates, so eat plenty of them. This has to be one of my favorite topics – the importance of fats. Dietary fat is vital in a PCOS diet as it slows the release of glucose, ensuring your blood sugar levels remain relatively stable. Fat can also be important in weight management as it helps you feel full and stops overeating. One fat you can safely cut out is trans fats, which are unhealthy and now banned in the US. Trans fat raises LDL cholesterol (the bad kind), while reducing HDL cholesterol (the good kind). Since you’re already at risk of diabetes, heart disease, and high cholesterol from PCOS, you don’t need to add to the risk by eating these fats. Then you can turn to other healthy fats, namely monounsaturated and polyunsaturated fats from nuts, seeds, and avocados. No discussion on fats can leave out the importance of omega 3 fatty acids. These essential fatty acids prevent or reduce symptoms of multiple conditions, and PCOS is no exception. They don’t just decrease cholesterol and lower blood pressure, but they have also been shown to be effective in improving hirsutism and insulin resistance in patients with PCOS. The Role of Exercise Physical activity has been shown to play an important role in the treatment and prevention of insulin insensitivity, meaning it’s key to the management of PCOS. At least 30 minutes of aerobic activity is recommended a week. Aim for strength training twice a week, as in order to improve insulin levels and aid weight loss, lifting weights is thought to be an important aspect of exercise for those with PCOS. In addition to regular exercise, eating whole grain carbohydrates, healthy fats, limiting sugar, and supplementing with vitamins in order to manage your PCOS, there are a few other things to consider.
Here’s an idea of what a typical day looks like on a PCOS friendly diet – pretty good wouldn’t you say? Just make sure to adjust your portion size based on your calorie needs.
Need help on finally losing that weight for good? If you would like help on figuring out your portion sizes for your specific goals, reach out to me and apply for a free, no pressure, 15 minute coaching call. During this call we will discuss your fitness and nutrition goals and see if I can help you see that success faster. -Coach Kayli |
AuthorKayli is a certified personal trainer and online coach that specializes in fitness, wellness, nutrition, mindset, mobility and everything in between. Categories
All
Archives
June 2024
|
Call Us 620-757-9146
Home | About Us | Personal Training | Online Nutrition and Fitness Coaching | Custom Training Plans | Breakfast | Entrees | Dressings | Snacks | Blog
Phoenix Rising Podcast | Product Recommendations | Contact Me
Phoenix Rising Podcast | Product Recommendations | Contact Me
Copyright 2024 Kayli Montoya Fitness

