Blog Post by Coach JulieNCI Certified Nutrition Coach L1 and Certified Mindset Coach Rheumatoid arthritis (RA) is a chronic autoimmune condition characterized by inflammation of the joints, leading to pain, stiffness, and swelling. While the exact cause of RA remains unclear, emerging research suggests a significant connection between gut health and the development or progression of this debilitating condition. In this article, we'll explore the intricate relationship between gut health and rheumatoid arthritis and discuss actionable steps to support gut health for potential RA management.
Understanding Gut Health: The gut microbiome, comprising trillions of bacteria, fungi, and other microorganisms, plays a crucial role in maintaining overall health. This diverse ecosystem not only aids in digestion and nutrient absorption but also influences immune function, metabolism, and even mental health. Gut Dysbiosis and Inflammation: Dysbiosis, an imbalance in the gut microbiota composition, has been implicated in various inflammatory conditions, including rheumatoid arthritis. Research suggests that dysbiosis may contribute to RA by promoting systemic inflammation and triggering autoimmune responses. Evidence of Gut-Joint Axis: Recent studies have uncovered a fascinating link between the gut and joint health, known as the gut-joint axis. This bidirectional communication pathway involves immune cells, microbial metabolites, and inflammatory mediators that can influence both gut and joint inflammation. Key Factors Influencing Gut Health and RA:
Clinical Studies and Insights: A growing body of research supports the gut-joint connection in rheumatoid arthritis. For instance, a study published in Nature Communications found that gut dysbiosis preceded the onset of arthritis symptoms in mice, highlighting the potential role of the gut microbiota in RA development. Another clinical trial demonstrated that probiotic supplementation improved RA disease activity scores and reduced inflammatory markers in patients with active disease. Conclusion: In conclusion, the relationship between gut health and rheumatoid arthritis underscores the importance of holistic approaches to disease management. By addressing gut dysbiosis through dietary modifications, probiotics, stress management, and avoiding gut irritants, individuals with RA can potentially mitigate symptoms and improve overall well-being. As research in this field continues to evolve, integrating gut-focused interventions into RA treatment plans holds promise for optimizing therapeutic outcomes and enhancing quality of life. References:
0 Comments
Blog Post by Coach JulieNCI Certified Nutrition Coach L1 and Mindset Coach Artificial sweeteners have been the bastard of the nutrition and fitness industry lately. They are getting the blame for cancer, gut health issues, disordered eating and blood sugar spikes. But what is the truth about artificial sweeteners.
The three most popular artificial sweeteners on the market today are: aspartame, sucralose, and saccharin. These sweeteners are often found in popular foods that have been reformulated into a “zero sugar” version which often results in a reduced calorie option of the popular alternative. For example, I enjoy Sprite Zero because it offers a “treat” with dinner for zero calories where a can of Sprite is about 120 calories. Sprite Zero contains aspartame to give it the sweet flavor without the calories mounting. These sweeteners have been on blast by the media about their “harmful” effects for years. The issue with media, is that it is almost always sensationalized to gather attention. Clicks and shares usually mean income for news media so you will often see stories overly sensationalized to garner more attention. You can see this very clearly in the amount of stories on news outlets about terrorism and violent crimes. It has created an attitude that the world is a super dangerous place, but actual studies have shown that crime has been down the last several years. The WHO (World Health Organization) came out a few years ago and said there MAY be a link between artificial sweeteners and cancer risk. This simple, yet uncertain claim has sparked the media firestorm that has created a line in the sand between nutrition researchers and cherry picking, media outlets that are trying to boost their bottom line. In an great article by Mike Matthews of Legion Athletics, Mike shows a great graphic on where the WHO categorized artificial sweeteners. He stated, “The WHO is placing aspartame in Group 2B. Thus, according to the WHO’s assessment, aspartame is about as likely to increase your cancer risk as aloe vera, carpentry, and eating pickled vegetables.” I’m not real sure about you, but if I find joy in one Sprite Zero per day, I feel relatively safe doing so. There have been recent studies lately that are showing that there is NO association between these sweeteners and cancer. In a recent news story on Barbend, the study has dispelled the WHO’s previous claims and actually shown that zero calorie sodas may be beneficial for health if it’s used to replace regular soda for weight loss because it aids in weight loss and reduces the overall sugar intake. The other big concern surrounding artificial sweeteners is their effect on gut health. There have been small sample studies done in rats on the effects of sweeteners on the gut microbiome. The issue is, rat studies don’t always translate well to humans. Most of these studies were feeding the rats toxic amounts of sweeteners that would translate to obscene numbers in humans. A recent article on StrongerU as well as an article on BioLayne, show the limitations associated with the rat studies. Overall, the studies on gut microbiome have been widely inconclusive. Some social media influencers have argued that these sweeteners promote obesity by increasing cravings. Here’s the thing, this argument also has no conclusive evidence of this. As a nutrition coach, I believe if you maintain a 80-20 diet in nutritious foods and use these zero calorie foods and drinks as a “treat” that subs for the higher calorie options, you’re going to be just fine. I don’t believe that these foods drive cravings more than any other food option. Realistically, this argument could be made about most highly processed, higher carb foods, they also tend to promote cravings because carbs do not offer the satiating effect you receive from protein. With all of the recent research, I’m not willing to tell any of my clients to stop choosing zero calorie sodas over regular sodas. I would caution that too much of any good thing can be a bad thing. The studies have not shown conclusive evidence of causing harm in small amounts. If you are drinking obscene amounts of these sweeteners, we need to have a different conversation because I would assume you’re having health issues. Those issues would be associated with dehydration NOT the artificial sweeteners. Overall, the benefits of artificial sweeteners far outweigh the potential risks, if used in a reasonable amount. Blog Post by Coach JulieNCI Certified Nutrition Coach L1 & Certified Mindset Coach A little bit of a change this week from my usual blog posts. This week I’d like to talk about stress and mindset. As I’m sure most of you know, Kayli’s dad passed away unexpectedly in July. This event just added to what would be the perfect storm for me, which ended up leaving me very sick and struggling with my mindset.
We lost Kayli’s dad on a Tuesday. The first week, I managed well. By managed I mean, Kayli had all the support she needed and wanted and a partner that was helping her navigate all the things that needed to be addressed. I knew that she would not be able to make a lot of decisions or absorb a lot of the information she was being given, so I stepped in and up and was all of those things for her. The problem was, I put myself on the back burner. I completely neglected my own needs. I was stressed. I was grieving, but I didn’t want her to see that part of me because I felt like it would make it worse for her. I was wrong. It ended up being worse for me. The second week, Kayli started to move through the stages of grief, but while she was starting to move forward, I was just starting to feel the sadness. Since I stifled my own grief, thinking I was helping her, I delayed my own emotions and left me sad and grieving when she was close to being done with that stage. The exact thing I hoped to avoid, happened. I didn’t want her to have to abandon herself to take care of me. Had we gone through this together and I would’ve been transparent with her about my emotions we could’ve leaned on each other rather than taking turns being each other’s leaning posts. Since Kayli spent the second week taking care of me, I felt really guilty that she was having to take care of me. My mindset tanked. I felt like a bad spouse. I felt weak. Things just kept spiraling. The process of having to manage all of the final affairs for Kayli’s dad lasted two and half weeks. That period of time was persistent high stress. Add in an insanely toxic and high stress environment at work and you have “the perfect storm.” I noticed on July 21st that I started having diarrhea that was difficult to control. I felt like I couldn’t control my bowels. I could, but I was not confident in that. The diarrhea, nausea, headaches and fatigue persisted. It is August 15th as I write this and I’m just now 2 days diarrhea free but not nausea free. It’s been going on that long. I’ve been to 3 doctors because I’m worried about my gut relapsing. Through the process of doctors visits, I was diagnosed with Hashimoto’s Thyroiditis, an autoimmune condition that causes your thyroid hormones to wax and wane. Hashimoto’s can be caused by chronic stress and leaky gut syndrome. All three doctors gave me the same unconventional response to help alleviate some of my symptoms, QUIT YOUR JOB. I was stuck. I couldn’t quit my job yet. Kayli and I just paid for a funeral and we have bills to pay for our home and our business. It just wasn’t feasible. I was stuck in a perpetual loop everywhere I looked. I was stressed so my gut was inflamed, but the gut inflammation and symptoms caused stress. Work stressed me out, but taking mental health days stressed me out because I knew what would be waiting on me when I got back. The cycles kept me in a doomsday mindset. I felt like nothing would get better. I felt terrible about myself. I started having OCD episodes of suicidal intrusive thoughts again. I was panicky all the time. I. COULDN’T. STOP. Finally, I got a break. On Monday morning at 6:30am I received a job offer asking when I could start. It was the miracle I needed. I accepted the offer and told my boss first thing that morning that I would be leaving effective this week. Suddenly the gut started to feel better. It isn’t perfect yet, it’s still a work in progress, but the gut isn’t where it was. The stress associated with my job had me stuck back in a chronically ill cycle that I hadn’t been in for years. Quitting my job and spending a week being intentional about my time with Kayli and enjoying our time were the meds that I needed. The take home here is, you have to manage stress. Sometimes you won’t be able to. That’s where I thought I was, but because I didn’t give up and I kept persisting even when things were hard, something shook loose. Stress can absolutely create a mess of your health if you don’t check it. Stay ahead of it. Had I stayed ahead of it, I may not be in this position. Learn from my mistakes. Blog Post by Coach JulieNCI Certified Nutrition Coach L1 & Certified Mindset Coach Antibiotics are one of the miracles of modern medicine. They have been used in phenomenal, life saving ways. When used sparingly and appropriately, antibiotics can be life changing. However, recently antibiotic use has become a quick fix solution to a multitude of conditions and issues in traditional, Western medicine. The use of antibiotics is not without its fair share of side effects. When used inappropriately, your body can become resistant to the positive effects of the drugs and they can cause side effects that can affect your health long term. While this is true for anyone, these long term effects can be more prevalent when antibiotics are used in children 3 and under.
Children under 3 are still developing the most important, beneficial bacteria in their gut that forms their microbiota. Studies have shown that antibiotic use early in life or mother’s antibiotic use during pregnancy or lactation can cause gut dysbiosis of the child. This dysbiosis can have several different effects on the child both short term and long term. The most common side effect of antibiotic use is diarrhea. While this is a more short term effect, it is the most obvious sign of microbiota disruption in children and adults alike. Research has shown that early use of antibiotics can have a direct effect on body weight. Studies have shown a correlation between this type of drugs and an increased BMI by ages 4-7. Interestingly, antibiotic use among young children has also been linked to immunity and food allergies. The studies have specifically noted that dairy allergies have been the most common type of food allergy in young children treated with antibiotics. Children that were breast fed by a mother who was treated with antibiotics during lactation also saw an increased risk for a dairy allergy, most commonly cow milk. Antibiotic use in infancy is also a risk factor for allergic rhinitis and early onset childhood asthma. Antibiotic use before one year of age had the highest risk of inflammatory bowel disease development. The risk, while still present, did decline through age 5. Studies show a correlation between early antibiotic use and type 2 diabetes, however it is unclear if the antibiotics were prescribed over time to treat symptoms of undiagnosed type 2 diabetes or if the antibiotic use was the catalyst. Studies are still suggesting that it is due to the use of antibiotics. Finally, and possibly the most concerning in my opinion, is that antibiotic use has been shown to increase the risk of certain types of cancers. The risk did increase with multiple rounds of antibiotics over time. Several cancers were listed. Among them: pancreatic, prostate, esophageal, gastric, lung and breast cancers. The point here is to not fear antibiotics. You should be mindful of the frequency and dosage of the medications. You should also just be aware and be educated. Awareness is key. Don’t walk blindly into anything. Ask questions. Your doctor should have your best interest in mind and should be happy to answer questions. If not, you may need a new primary care physician. Blog Post by Coach JulieNCI Certified Nutrition Coach L1 & Certified Mindset Coach You’re probably a little confused right now . . . Let me break it down for you.
I have clients that struggle terribly with allergies and asthma. They’ve tried everything. Expensive allergy testing shows no allergies. NONE. Believe it or not, the problem may not be allergies, it may be issues with the gut. It may sound crazy that your gut health would affect your sinuses, but the two systems are very intertwined. Both the respiratory tract and the digestive tract are immune barriers, meaning it’s their job to protect the body from outside invaders. The gut in particular profoundly influences the entire immune system. When gut health suffers so does the rest of your body. This can even result in allergy symptoms that flare up each spring. Leaky gut, also known as intestinal permeability, is a condition in which the lining of the digestive tract becomes inflamed and porous, allowing undigested foods, bacteria, yeasts, and other toxins into the bloodstream. The immune system launches an attack on these toxins, which creates inflammation throughout the body. For many people, this happens every time they eat. This inflammation manifests in different ways for different people. Gut symptoms don’t have to be present to suffer from inflammation caused by leaky gut. It can cause joint pain, skin problems, digestive complaints, autoimmune disease, issues with brain function, fatigue, chronic pain, asthma, and…seasonal allergies. Chronic stress also weakens and inflames the digestive tract, causing leaky gut. Stress doesn’t just have to come from a stressful lifestyle or lack of sleep, although those certainly play a role. Eating a diet high in sugar, fried and processed foods is stressful to the body, as is an unmanaged autoimmune disease, or hormones that are out of whack. These are just a few metabolic factors that can contribute to leaky gut. If you need help managing chronic conditions or gut health, shoot Coach Kayli or I a DM. We’d be happy to jump on a coaching call with you to discuss your issues and help you get to the root cause. Blog Post by Coach JulieNCI Certified Nutrition Coach L1 & Certified Mindset Coach  Do you suffer with Rheumatoid Arthritis? Rheumatoid arthritis (RA) is an autoimmune and inflammatory disease. Symptoms of this disease are tender, warm or swollen joints, joint stiffness, fatigue, fever and loss of appetite. Early symptoms tend to appear in the smaller joints first, usually hands and feet. RA symptoms can wax and wane in severity including periods of remission and alternatively periods of increased intensity, called flared. Long term effects of this disease can cause your joints to deform and shift out of place. Western medicine admittedly states they are not sure what causes RA. They state they believe there is a genetic component, but that genes don’t actually cause the issue. This is something that I have been trying to teach my clients and audience, genes don’t cause or create a diseased state in your body. Just because your parents have diabetes does not mean that you’re doomed to have diabetes. If that’s how disease worked, you would have diabetes when you were 7. It wouldn’t wait until you were 37. Genetics may make you more predisposed to a certain disease or condition, but environmental factors have to be present to trigger and activate that disease. Your genetics load the gun, but your lifestyle and environment pull the trigger. This is why it is important to manage your health and wellness throughout your life and prior to symptoms appearing. Usually if you wait for symptoms to appear, the disease is already present. Studies are suggesting that there may be a link between Rheumatoid Arthritis (RA) and gut health. I can’t say that I’m surprised by this. RA is an autoimmune disease and an inflammatory disease. The root cause of many autoimmune diseases is inflammation and inflammation usually comes from the gut. This is where the environmental factors we spoke about above come into play. These studies are specifically referring to low stomach acid causing flares of RA. When stomach acid is low, usually people will experience food-allergy symptoms which can show up as RA pain. Stomach acid helps break down proteins in your stomach so that the intestines can absorb it. Without adequate stomach acid, your intestines absorb partially broken down protein which causes allergies. Signs of low stomach acid are: abdominal pain, bloating, gas, diarrhea, constipation, undigested food in stool, reflux and heartburn. Yes, you read that right, reflux and heartburn are signs of low stomach acid, not too much acid. If you struggle with RA, you may see some relief by looking at your gut health and working to optimize gut health. Avoid proton pump inhibitors (PPIs) like Prilosec or Nexium as they will lower your stomach acid. Some RA sufferers have stated that there are RA drugs that have caused acid reflux issues and therefore they have been prescribed a PPI to help them manage. It is very important to talk to your doctor about other options. Perhaps a change in your RA medication would be an option. If not, I would suggest doing some stomach acid tests to see if the issue you are experiencing is actually high stomach acid. If it isn’t, you have other options. If you are experiencing low stomach acid, you could find relief from your stomach acid issues but supplementing with Betaine HCL and adding stomach acid to your gut to help you break down food. This would not only eliminate the PPI and the symptom, but it would help you break down food and could potentially lessen the frequency and intensity of RA flares. What is PCOS - Polycystic Ovary Syndrome is a hormonal disorder that affects millions of women.2/4/2023 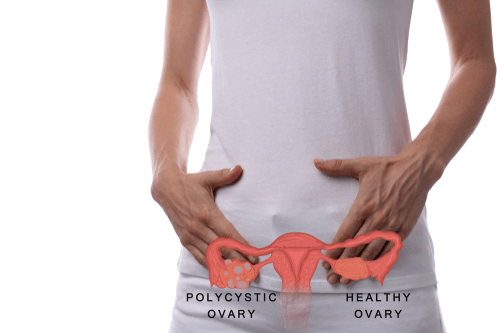 Polycystic ovary syndrome (PCOS) is a condition affecting between 1 in 10 and 1 in 20 women of childbearing age. This condition causes the body’s hormones to become unbalanced, leading to issues like ovarian cysts, increased hair growth on the face and body (hirsutism), acne, weight gain or obesity, thinning hair, irregular menstrual periods, and even infertility. It’s very likely you or someone you are close to suffers from PCOS. You must have two of the three following criteria to be diagnosed with PCOS : Irregular Periods Hyperandrogenism (Higher Testosterone) Polycystic Ovaries About 50% of people who have PCOS also suffer from obesity. Being diagnosed with PCOS is not a “death” sentence when it comes to being able to lose weight. Thankfully, more and more doctors are beginning to recognize the importance diet plays in preventing and controlling PCOS. Insulin is thought to play a major role in PCOS. This powerful hormone, released by the pancreas, exists to transport sugar out of the blood and into the cells. However, many women with PCOS are insulin resistant, meaning this process doesn’t work correctly within their bodies. As a result, high levels of insulin contribute to many of the symptoms of PCOS, such as weight gain, high cholesterol, diabetes, and ovarian cysts. Ladies, you’ll be glad to hear that controlling your diet can play a huge part in helping reverse insulin resistance. Firstly, stick to a balanced diet consisting of whole grains, fruit and vegetables, healthy fats, and protein. Losing just 5% to 10% of body weight can improve symptoms of PCOS and reduce insulin resistance. Physical activity has been shown to play an important, if not essential, role in the treatment and prevention of insulin insensitivity, meaning it’s central to the management of PCOS. At least 30 minutes of aerobic activity is recommended a week. Aim for strength training twice a week, as in order to improve insulin levels and aid weight loss, lifting weights is thought to be an important aspect of exercise for those with PCOS. Let’s have a look at the best dietary choices to decrease insulin resistance and therefore manage PCOS symptoms. While standard guidelines recommend that we get 45% to 65% of our daily calories from carbohydrates, women with PCOS should strive for the lower end of this range. If you’re already insulin resistant, a lower carb diet is typically a better option. I promise you won’t have to starve yourself to get the benefits of a lower carbohydrate intake. Even switching to a diet consisting of 43% carbohydrates has been shown to reduce fasting insulin levels, and therefore improve insulin sensitivity, in women with PCOS. Choose high fiber, whole grain carbohydrates like brown rice, oatmeal, whole rye, and whole wheat pasta in small amounts. Not only do whole grains have a lower GI rating, which improves insulin sensitivity, but they also help improve cholesterol levels – another PCOS-related complication. And don’t forget the vegetables. These are always your best source of carbohydrates, so eat plenty of them. This has to be one of my favorite topics – the importance of fats. Dietary fat is vital in a PCOS diet as it slows the release of glucose, ensuring your blood sugar levels remain relatively stable. Fat can also be important in weight management as it helps you feel full and stops overeating. One fat you can safely cut out is trans fats, which are unhealthy and now banned in the US. Trans fat raises LDL cholesterol (the bad kind), while reducing HDL cholesterol (the good kind). Since you’re already at risk of diabetes, heart disease, and high cholesterol from PCOS, you don’t need to add to the risk by eating these fats. Then you can turn to other healthy fats, namely monounsaturated and polyunsaturated fats from nuts, seeds, and avocados. No discussion on fats can leave out the importance of omega 3 fatty acids. These essential fatty acids prevent or reduce symptoms of multiple conditions, and PCOS is no exception. They don’t just decrease cholesterol and lower blood pressure, but they have also been shown to be effective in improving hirsutism and insulin resistance in patients with PCOS. The Role of Exercise Physical activity has been shown to play an important role in the treatment and prevention of insulin insensitivity, meaning it’s key to the management of PCOS. At least 30 minutes of aerobic activity is recommended a week. Aim for strength training twice a week, as in order to improve insulin levels and aid weight loss, lifting weights is thought to be an important aspect of exercise for those with PCOS. In addition to regular exercise, eating whole grain carbohydrates, healthy fats, limiting sugar, and supplementing with vitamins in order to manage your PCOS, there are a few other things to consider.
Here’s an idea of what a typical day looks like on a PCOS friendly diet – pretty good wouldn’t you say? Just make sure to adjust your portion size based on your calorie needs.
Need help on finally losing that weight for good? If you would like help on figuring out your portion sizes for your specific goals, reach out to me and apply for a free, no pressure, 15 minute coaching call. During this call we will discuss your fitness and nutrition goals and see if I can help you see that success faster. -Coach Kayli Blog Post by Coach JulieNCI Certified Nutrition Coach L1 & Certified Mindset Coach I began Phase 5, the Nexium cessation phase on December 2nd. With this phase, I am moving through what was supposed to be a 4 week titration phase off of Nexium. We are currently on Week 6 of this process, which means I have definitely hit some snags and we needed to slow the process down. This is perfectly normal. Some people can complete the process in 4 weeks and others need more. Since I’ve been on this medication for 15+ years, I require some more.
During this phase, I have continued to take Zinc Carnosine at 75mg every morning on an empty stomach. I have also continued to take peppermint oil capsules before my morning and evening meals. Zinc carnosine reduces gut inflammation and helps protect the gut lining, which will be integral while my gut acid levels increase to their normal levels after being repressed for so long. Peppermint oil soothes the gut and helps prevent cramping and discomfort. I have also added DGL chewables and Betaine HCL. The DGL chewables are taken after my morning and evening meals. 3 tablets after each meal. The DGL chewable is Deglycyrrhizinated Licorice Root. I have used this supplement in a capsule form earlier in my journey. DGL is often used to soothe the stomach and support healthy digestion by encouraging mucin production. The Betaine HCL will be added in as needed, but I have not needed it yet. Betaine HCL helps protect the gut wall and strengthens it throughout the process. It will also help increase your stomach acid levels when you are struggling to recover with low stomach acid, which is common after long term use of a PPI. I will be using it as needed should I begin having acid reflux symptoms. After week one of this process, the withdrawal symptoms started. Week one consisted of reducing my Nexium to every other day rather than daily. After about day 4, I began noticing some mild diarrhea and headaches. I also noticed some weakness and dizziness. I am also having some reflux which is a most common and expected side effect. The reflux has been causing some nausea for me. Based on this, rather than moving to week 2, we decided to repeat week 1 again to see if my body would adjust. I continued to have symptoms so we decided to repeat week 1 for a third week to see if my body adjusted to the titration. My gut did regulate during the last 2 weeks of that process, so I then moved the Nexium to once every two days. I didn’t notice any reappearance of symptoms every two days, so I progressed to once every 3 days to see how my body tolerated that before we completely stopped the PepZin GI and the Nexium. After no noticeable symptoms or side effects, I took my last Nexium tablet on January 11th. Subsequently, I took my last PepZin GI tablets on January 13th. I have noticed that some meals seem to cause a slight acidic feeling in my gut. It does not feel like full heartburn or acid reflux, just a sensation that I am acutely aware of and it is manageable. One noticeable change was my bowel movements became more regular and more normal. This was something that I have not experienced in many years. Even after healing my gut I was still having a bit of constipation and this was apparent in the frequency and consistency of my bowel movements. On January 16th, I had a day of terrible heartburn. This was the first time that I have struggled with it since we started the process. The heartburn persisted for most of the week. On Tuesday, I decided to go ahead and try Betaine HCL with dinner to see if it would help. I noticed a reduction of the acidy, burning feeling shortly after taking it. The next morning I took another with my protein shake. I believe I may have taken it too soon because I felt very ill the rest of the morning. I struggled with reflux and nausea. Betaine HCL should be taken in the middle of your meal or immediately after your meal for the best effectiveness. If taken too soon or before a meal, you can get a false heartburn feeling. I took the Betaine HCL after only one drink of my protein shake and I believe this to be the cause. That same day after I ate lunch, some of the symptoms seemed to subside a little. The following day, I waited until my protein shake was complete before taking the Betaine HCL. I noticed the symptoms were greatly improved and easy to manage. It does seem that the Betaine HCL is helping increase my stomach acid levels and which is keeping the reflux to a minimum. I have noticed as the weeks progressed that my bowel movements became more regularly occurring. They also seemed to be moving toward the normal range on the Bristol Stool Scale. As always, I will provide a case study update in 4 weeks, when I should have completed this final phase if my body responds well. My body has responded exceptionally well the last few months so I am hopeful this temporary struggle will be the last and I will bounce back to normal. Blog Post by Coach JulieNCI Certified Nutrition Coach L1 & Certified Mindset Coach I began Phase 4, the reintroduction phase, on July 7th. With this phase I started 2 new supplements Flora Protect and a supplement called PepZin GI. These two supplements are to repopulate the gut with good bacteria and to protect the gut barrier and gut immunity. I will maintain the S. Boulardii with these two supplements and I have continued the peppermint oil. I am reintroducing foods on a 3 day cycle. The first day, I will consume half a serving of a certain food. If I don’t have symptoms, I will continue to day two where I will consume a half serving twice per day. Assuming there are still no symptoms, I will eat a normal serving on day 3. Day 4 is a rest day, to make sure that I don’t experience any delayed symptoms. Sometimes delayed symptoms can occur if you’re experiencing constipation so we’ve built in a rest day to allow any symptoms to subside before we start a new 3 day cycle with a different food. After the end of the cycle, if there were no symptoms, I have been waiting a week or so and then reincorporating those foods back into my normal diet. Since the last update, I have reintroduced: salsa, amino energy (inulin) and alfredo. All have been a successful introduction. There were no noticeable symptoms with any of those items. Upon the completion of the 3 day cycle for these remaining foods, I had successfully completed a 21 week reintroduction phase. I did not have any foods that stood out as terrible triggers for my gut. I had some questionable issues with garlic, however I believe those to be dose dependent. This Phase ended on November 29th. I have discontinued all the supplements, including S. Boulardii, with the exception of the PepZin GI and Peppermint Oil. I will be continuing those through Phase 5, the Nexium cessation phase. We have now moved onto Phase 5, effective December 2nd. During this phase, I will move through a minimum 4 week phase where I titrate off of Nexium to discontinue its use. Long term use of a PPI (proton pump inhibitor) can be very detrimental to your health. You should be using these PPIs (Nexium, Prilosec, etc) for 3 weeks at the most to treat a temporary flare up. Long term use of PPIs can lead to increased risk of cancer, risk of fractures, pneumonia, Clostridium difficile diarrhea, hypomagnesemia, vitamin B12 deficiency, chronic kidney disease, and dementia. If you have been using these medications long term, you should not stop abruptly. You should use a step down method to gradually decrease your dose. I have been taking Nexium for over 15 years so the process will take at least 4 weeks, but could potentially last longer. During this phase, I will continue to take Zinc Carnosine at 75mg every morning on an empty stomach. I will also continue to take peppermint oil capsules before my morning and evening meals. Zinc carnosine reduces gut inflammation and helps protect the gut lining, which will be integral while my gut acid levels increase to their normal levels after being repressed for so long. Peppermint oil soothes the gut and helps prevent cramping and discomfort. I will also be adding in DGL chewables and Betaine HCL. The DGL chewables will be taken after my morning and evening meals. 3 tablets after each meal. The DGL chewable is Deglycyrrhizinated Licorice Root. I have used this supplement in a capsule form earlier in my journey. DGL is often used to soothe the stomach and support healthy digestion by encouraging mucin production. The Betaine HCL will be added in as needed. Betaine HCL helps protect the gut wall and strengthens it throughout the process. I will be using it as needed should I begin having acid reflux symptoms. After week one of this process, the withdrawal symptoms started. Week one consisted of reducing my Nexium to every other day rather than daily. After about day 4, I began noticing some mild diarrhea and headaches. I also noticed some weakness and dizziness. I am also having some reflux which is a most common and expected side effect. The reflux has been causing some nausea for me. Based on this, rather than moving to week 2, we decided to repeat week 1 again to see if my body would adjust. I continued to have symptoms so we will repeat week 1 for a third week to see if my body adjusts to the titration before moving to the next step of the process which will be reducing Nexium to once every two days. Withdrawal symptoms from a PPI are common, especially after long term use. Symptoms frequently include acid reflux and indigestion. There are, however, less common side effects that include: anxiety, depression, diarrhea, nausea, vomiting, constipation, headaches, dizziness and more. As always, I will provide a case study update in 4 weeks, when I should have completed this final phase if my body responds well. My body has responded exceptionally well the last few months so I am hopeful this trend continues. Blog Post by Coach JulieNCI Certified Nutrition Coach L1 & Certified Mindset Coach I began Phase 4, the reintroduction phase, on July 7th. With this phase I started 2 new supplements Flora Protect and a supplement called PepZin GI. These two supplements are to repopulate the gut with good bacteria and to protect the gut barrier and gut immunity. I will maintain the S. Boulardii with these two supplements and I have continued the peppermint oil. I am reintroducing foods on a 3 day cycle. The first day, I will consume half a serving of a certain food. If I don’t have symptoms, I will continue to day two where I will consume a half serving twice per day. Assuming there are still no symptoms, I will eat a normal serving on day 3. Day 4 is a rest day, to make sure that I don’t experience any delayed symptoms. Sometimes delayed symptoms can occur if you’re experiencing constipation so we’ve built in a rest day to allow any symptoms to subside before we start a new 3 day cycle with a different food. After the end of the cycle, if there were no symptoms, I have been waiting a week or so and then reincorporating those foods back into my normal diet.
Since the last update, I have reintroduced: ranch dressing, granola, avocado, ice cream, pears, beets, onion and garlic. All have been a successful introduction. The only noticeable symptoms I have had occurred during the garlic reintroduction. I had minimal stomach upset and a little bit of a bloated feeling. Not enough that I will completely exclude garlic, but I will keep it to a minimum. I am still working through a list of foods that I had eliminated and this will continue until I have tried all the foods that I eliminated so that I am either back to a normal diet or have identified some trigger foods. I am getting very close to wrapping this phase up, I have 3 more foods that I would like to add. I am taking this phase very slowly to be sure that I can clearly identify if there are some trigger foods. My coach has said that I can probably wrap it up, but I feel more comfortable maintaining this cadence until everything I used to eat is included. I have discontinued all the supplements, including S. Boulardii, with the exception of the PepZin GI and Peppermint Oil. I will be continuing those through the Nexium cessation phase. After this phase, we will move on to Phase 5 where we will eliminate Nexium and work on increasing my stomach acid levels. I have the protocol and I know what I will be adding, however I am not going to start this until I have completed the current supplementation and the reintroduction phase. With my forecasting, it looks like I will be starting that phase on December 3rd. |
AuthorKayli is a certified personal trainer and online coach that specializes in fitness, wellness, nutrition, mindset, mobility and everything in between. Categories
All
Archives
June 2024
|
Call Us 620-757-9146
Home | About Us | Personal Training | Online Nutrition and Fitness Coaching | Custom Training Plans | Breakfast | Entrees | Dressings | Snacks | Blog
Phoenix Rising Podcast | Product Recommendations | Contact Me
Phoenix Rising Podcast | Product Recommendations | Contact Me
Copyright 2024 Kayli Montoya Fitness

